Dealing with Autosomal Dominant Polycystic Kidney Disease (ADPKD)
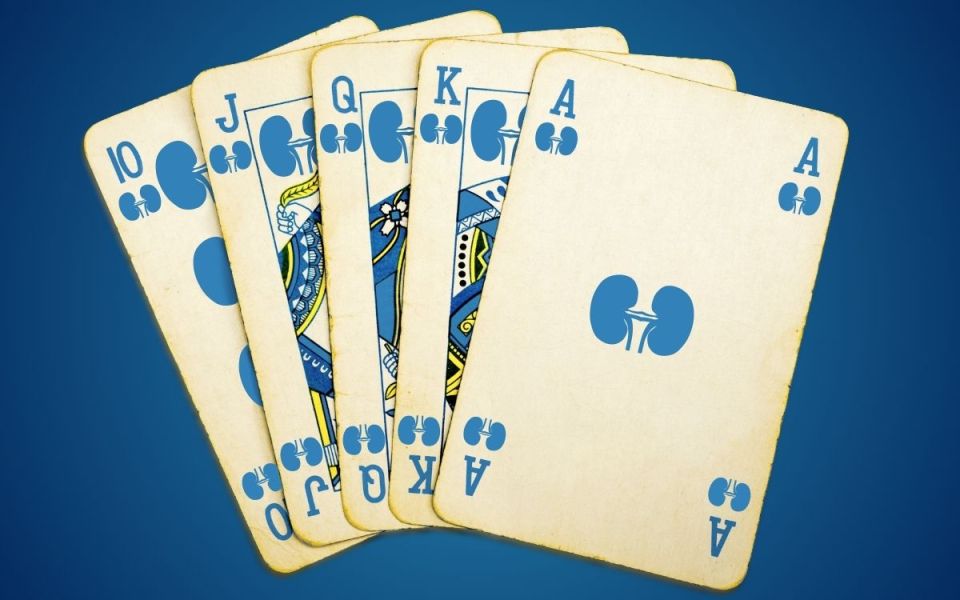
I’ve been playing a lot of cards lately, and sometimes you just get dealt a crap hand. Of course, the responsible thing is to fold, but sometimes you just have to hang on and hope something lucky will come down the river. Progressive genetic diseases can feel like this as well. Your genes determine how some diseases will develop over time, and there’s not much you can do but hold on and hope science comes up with a solution. With autosomal dominant polycystic kidney disease, good cards are starting to show and hope may come with successful clinical trials.
Autosomal dominant polycystic kidney disease (ADPKD) is the most common hereditary kidney disease, but is still rare, affecting only 1 in every 1,000 to 2,500 people.[1] It is a genetic disorder where a single mutated gene causes fluid-filled cysts to form in the kidneys before birth.[2] Over time, these cysts fill with fluid, causing the kidneys to grow from the size of a fist to that of a football, which damages kidney tissue and impairs its function.[2,3,4] Because cysts take time to grow and the kidney compensates for damage, many patients have no signs or symptoms until their late thirties or beyond.[3] By age 70, a majority will need assistance with their kidney function,[5] but as Dr. Chebib states on the MedEvidence Podcast:
“It's considered a relatively good prognosis in general…our ADPKD patients, if they have healthcare and they take good care of themselves, they should live a normal life.”[3]
Genes determine who gets ADPKD… but how? Two genes, PDK1 and PDK2, encode proteins that change signaling pathways.[5] These genes are active before birth in kidney cells and are responsible for normal cell processes like fluid transport, cell specialization, forming new cells, cell death, and attaching to neighboring cells.[5] When a fetus has the dangerous forms of PDK1 or PDK2, cells errantly form the tiny, fluid-filled cysts characteristic of ADPKD.[5] The exact mechanisms for how the cysts form and grow are complex, but include signaling molecules, immune cells, and enzymes.[6] Disrupting these activities may cause the cysts to metaphorically fold and slow the progression of ADPKD.[6]
Slowing cyst growth is a good bet for good outcomes, as pushing the need for kidney assistance from ~70 years old to over 100 would make the drawbacks of this disease moot. Large cysts damage the kidney’s main function, which is to filter blood.[1] Cysts can also cause abnormal connections among cells, metabolic changes, increased blood pressure, kidney stones, and damaging inflammation.[1,2,5] Stacking on this, the cysts can become infected or rupture, causing pain and/or blood in the urine.[3] Outside of the kidneys, increased blood pressure and decreased kidney function can deal downstream damage, including to the heart, brain, and liver.[2,4]
This may sound like a wild amount of problems, but doctors and scientists have been raising our ability to slow cyst growth and mitigate ADPKD’s effects. The king of ADPKD management is a healthy lifestyle, including:[2,3,4]
- Extra water; aiming for between 100 oz and 1 gallon per day
- Less salt; under 2.3-3 grams per day
- Moderate amounts of protein; between 0.8 and 1 grams of protein per kilogram of bodyweight (~60 grams for a 150-pound person)
- Maintaining a healthy weight; moderating calories and aiming for a “Normal” BMI
- Quitting smoking
- Exercise
Beyond lifestyle changes, medications can chip in to help. Keeping blood pressure under control is very important, and maintaining healthy cholesterol levels is recommended.[4] Doctors may also prescribe the only currently FDA-approved medication, tolvaptan, also called Jynarque. This suppresses one of the critical signaling molecules involved with cyst growth, helping to slow the progression of the disease and protect kidney cells.[2,3,4] Side effects and drug-to-drug interactions make tovaptan difficult for many patients to tolerate, so new therapies are a high priority.
Luckily, the ace in the hole for ADPKD patients is clinical trials, which are drawing new treatments closer than ever. On the near horizon, medications targeting cyst growth are expected to enter clinical trials soon.[3] A little further out, treatments are looking at solving the underlying genetic issues caused by faulty PDK1 and PDK2 genes.[3] When combined with disease-altering medications and a healthy lifestyle, clinical trials will leave ADPKD patients flush with treatment options. What a deal!
Creative Director Benton Lowey-Ball, BS, BFA
|
Click Below for ENCORE Research Group's Enrolling Studies |
|
Click Below for Flourish Research's Enrolling Studies |
References:
[1]Cornec-Le Gall, E., Alam, A., & Perrone, R. D. (2019). Autosomal dominant polycystic kidney disease. The Lancet, 393(10174), 919-935. https://www.proquest.com/docview/2186986383?accountid=14690
[2]Jdiaa, S. S., Mustafa, R. A., & Alan, S. L. (2025). Treatment of autosomal-dominant polycystic kidney disease. American Journal of Kidney Diseases, 85(4), 491-500. https://www.sciencedirect.com/science/article/pii/S0272638624010321
[3]Koren, M. J., Chebib, M. (16 July, 2025). What's on the horizon for polycystic kidney disease (PKD)? On MedEvidence! Truth Behind the Data. [Podcast]. https://medevidence.com/whats-on-the-horizon-for-polycystic-kidney-disease-pkd
[4]Chebib, F. T., & Torres, V. E. (2018). Recent advances in the management of autosomal dominant polycystic kidney disease. Clinical Journal of the American Society of Nephrology, 13(11), 1765-1776. https://pmc.ncbi.nlm.nih.gov/articles/PMC6237066/
[5]Reiterová, J., & Tesař, V. (2022). Autosomal dominant polycystic kidney disease: from pathophysiology of cystogenesis to advances in the treatment. International journal of molecular sciences, 23(6), 3317. https://www.mdpi.com/1422-0067/23/6/3317
[6]Kashyap, S., Zeidler, J. D., Chini, C. C., & Chini, E. N. (2020). Implications of the PAPP-A-IGFBP-IGF-1 pathway in the pathogenesis and treatment of polycystic kidney disease. Cellular signalling, 73, 109698. https://www.sciencedirect.com/science/article/abs/pii/S0898656820301753